A Story About Anxiety
Written by PQ Miller
In Collaboration with JQ Miller
Dedicated to Lois Miller
Part 1
Chapter I
My story begins the year I turned 39, when I made the life-changing decision to have my first—and, as fate would have it, only—child.
My husband, Jim, was a high school math teacher, and I managed our custom picture-framing and art consulting business in the studio of our home.
We were like two kids in a candy store as we embarked on this new adventure of raising our first child together. Neither one of us had ever pictured ourselves as parents, especially after spending much of our younger years vowing never to do so. However, love has a way of changing your perspective on life.
For two people raised in the 1950s, it was common to be married and well on your way to having children by your mid-20s. But Jim and I both waited until the time was right for us, and now adding an adorable baby girl to our already blessed life was like putting a cherry on top of it.
Our daughter arrived nine months later, healthy and vibrant, filling our home with love and joy. We chose the name Jamie after her father’s formal name, James.
With my family of three, I had everything in life I could ever want and never been happier.
But as the wicked old saying goes, “Nothing lasts forever,” so it was with my beautiful little family.
Chapter 2 Nothing Lasts Forever
One morning, five months after Jamie was born, a snow emergency caused Jim's school to close; unfortunately, he had already left for work, missing the notice that classes were canceled.
He left earlier than usual, anticipating the poor road conditions he knew he would be facing. Since this was before having the convenience of cell phones, I had no way of letting him know.
Knowing Jim would be returning home soon, I went ahead and showered, getting ready for the day.
When the phone rang, I recall having a sinking feeling in my stomach as I walked over and picked up the receiver. On the other end, a doctor from an emergency room told me that my husband had been in an accident. He was halfway to the school when a young man, a high-risk driver, went left of center and hit Jim’s car head-on.
He spoke so quickly that I was finding it difficult to absorb everything he was saying, but I did hear the words, “He has severe injuries.”
Because of the urgency in the doctor’s voice, I finally asked, “Doctor, are you saying my husband is going to die?”
There was a pause, and then the doctor said, “There’s a possibility he may not make it.”
He continued to tell me that they were life-flighting him to a hospital that had a bypass machine to treat the life-threatening injuries he had received to his heart.
I hung up, and in desperation, immediately called my sister, who thankfully lived nearby. She, in turn, called a second sister, and both were at our home within 20 minutes. My niece was with them and volunteered to stay with Jamie.
The three of us jumped in the car and headed to the large metropolitan hospital 40 minutes away, where they were transporting Jim.
All I could think about on the way to the hospital was that I was certain Jim would be alright. Years ago, I had lost the young man I had been dating and planning to marry in a car accident. I thought to myself, surely something like this couldn’t be happening again.
When we arrived at the hospital, a nervous staff member couldn’t answer my questions about Jim’s whereabouts. She kept glancing toward the hallway, clearly waiting for someone to come and explain something she didn’t want to say.
When a nurse arrived, I asked in an anxious voice, “Where is my husband?” Looking very uncomfortable, she replied, “They took him back to the first hospital.”
She went on to explain that as they were loading up Jim for transport, his heart had gone into atrial fibrillation. I finally forced myself to ask the cold, hard question: “Is he dead?”
A heavy silence passed between us.
Then she answered softly, “Yes. Do you want to speak with someone from the hospital staff?”
I nodded yes, and she dialed the number, handing me the receiver. A woman on the other end of the line confirmed, “Yes, he’s here. Do you want to come and see him?”
The only thing I could say was, “No, it would break my heart.” She said, “Are you sure?” and I repeated again, “No, it would break my heart.”
I hung up the phone and turned around to find my two sisters, who had heard the conversation, standing there with tears in their eyes. My eyes were dry, but I was aware of a strange, low buzzing sound that had come into my ears. It was as if my senses were shutting down, incapable of accepting the reality of what was happening to me in that moment.
Chapter 3 Continuing On
When I arrived back home, it was a Thursday. The urgent need to arrange Jim’s burial weighed heavily on me. I needed to get back to raising our daughter as soon as possible, and knowing the challenges laying ahead would be unlike anything I had ever faced before.
I was determined to get us both through it.
Three days later, we had the funeral. It was done. Luckily, I was unaware of the difficult months and years that lay ahead of me. If I had known what was coming, I’m sure I would have struggled to find the courage to go on.
That first year, I was kept busy dealing with the wrongful death suit involving my husband’s accident and the added burden of taking on all the extra responsibilities in our lives that Jim had usually taken care of.
Jamie was a little trooper. In the days following her father’s death, I give her all the credit for getting up at six every morning. In the beginning, I went through each day feeling like it was all a bad dream.
I often found myself grappling with the reality of the situation, and on days when I worked in my studio, I would tell myself it was like any other day before his death; Jim was simply away at work.
As time passed, the pain of loss didn’t lessen; I just got better at living with it. The years slipped by as the usual milestones in Jamie’s life came and went, and her easygoing disposition made it such a pleasure raising her.
On her first birthday, we came from the grocery store. I placed her in the high chair and set a birthday cake in front of her. I watched with delight as she grabbed handfuls of cake and icing, eagerly eating and smearing it all over her face.
What should have been a joyous, memorable occasion was bittersweet for me. We were alone in our kitchen, just the two of us. As I took pictures to commemorate the moment for her scrapbook, I held back tears, deeply missing Jim for not being there to witness these precious moments in his daughter's life.
When Jamie was old enough to understand what Christmas was all about and the excitement of waiting for Santa Claus, I took her to a local Christmas tree lighting ceremony. I remember the deep sadness I felt as I watched all the other excited children with their parents, especially one child in particular, who was sitting on his daddy’s shoulders. I don’t need to tell how it was hard watching Jamie grow up without her wonderful father.
Chapter 4 The First Sign
Jamie and I settled into a normal family life, and as time went on, the loss of Jim began to ease. Now, I only experience deep sadness occasionally whenever a memory would pop up unexpectedly, reminding me of our loss.
In first grade, Jamie’s teacher asked the class to draw a picture of their family. When I saw Jamie’s, it was a drawing of me, her, and the two cats we had at the time. Of course, it saddened me that Jim was not in the picture, but then I had to admit we did treat the cats like family, even making sure they both had a gift under the tree at Christmas.
I kept that family drawing, and whenever Jamie and I run across it, we both laugh because I have always teased her, saying the old white cat who lived to be seventeen had helped raise her.
I was successful in running my business, and Jamie enjoyed school and spending time with her friends. Motherhood suited me; I loved it. My life felt complete, and if I had any regrets, it was, “Why didn’t I do this sooner?”
We engaged in all the usual fun family activities: trips to the beach, dance recitals, soccer games, and so on. I attempted to make every holiday memorable and worked hard to give Jamie the life that Jim and I had planned for her. However, there was one incident that, at the time, I didn’t realize as being that significant until much later.
One morning in fourth grade, while getting on the school bus, Jamie realized she had forgotten her lunch. Calling to the bus driver to stop, she came running back to the house. When I went to hand her lunch, she suddenly burst into tears, saying she couldn’t go to school. I could see that she was inconsolable in the moment and motioned for the bus driver to go on. Seeing the state she was in, I decided to let her stay home for the day.
Since it was still early, I told her we could return to my bed, snuggle for a while, and watch TV. When we got into bed, Jamie began trembling all over. Of course, I was concerned. I had never seen her like this before, and held her until she calmed down.
I didn’t understand what had happened, but as the day went on, she appeared to have recovered from her morning upset. We returned to our regular routine the following day, putting the previous day’s bus experience behind us.
I assumed the school bus incident was an isolated incident. Jamie had always been a sensitive child, and up until now, what behavior I had observed in her appeared normal for most children her age. However, with that being said, everything I had experienced in life up until now had not prepared me for what lay ahead…waiting for us.
Chapter 5
Later that same year, Jamie joined the school’s orchestra and began playing the violin. After attending classes for a few weeks, she started coming home distressed over her hands.
She had observed that the other children’s hands were larger than hers, and her fingers were stubbier. I sat and talked with her, assuring her that her hands were normal, explaining that it is perfectly normal for everyone to be a little different. But a week or so later, she came home again, upset over her stubby, short fingers. Again, we sat and talked until she calmed down.
This scenario repeated itself a few more times throughout the rest of the school year. Still, I wasn’t too concerned; I could always calm her down and remind her how well she played the violin, having already achieved the first chair second violin position. This phase she was going through didn't worry me. I knew it was around this age when children begin competing and comparing themselves to their peers.
During the next couple of years, nothing much out of the ordinary happened. We had moved to a new neighborhood, and Jamie was busy in school, sports, and discovering video games.
Saturday night was movie night at the Miller’s. We both enjoyed the latest releases, and Jamie, from a very young age, always showed a strong interest in moviemaking. She enrolled in a local film class and began having fun making home movies with her friends.
Chapter 6 The Day Everything Changed
When Jamie turned 13 and entered 7th grade, everything seemed to change overnight. It all began one day, picking her up from school; she climbed into the car and immediately began crying hysterically. She said the thoughts she was having about the other students scared her, and she felt overwhelmed by her inability to stop them. This was what I called her first ‘meltdown.’
It was the first time that ‘talking out’ her thoughts and feelings didn’t help calm her down. I can only describe the situation as an out-of-control mental storm that eventually wore itself out later that evening, leaving her exhausted.
I was terrified at what I had witnessed and recognized that something was seriously wrong with my daughter. I immediately sought help from our family physician.
The doctor listened as I described Jamie’s behavior and agreed it was not normal. She thought Jamie could be experiencing some form of anxiety and gave me a referral for her to see a child psychiatrist.
The very next week, we met with the psychiatrist. She was friendly, sort of a grandmother type. She interviewed Jamie and listened to my concerns. At the end of our consultation, she diagnosed Jamie with GAD (generalized anxiety disorder). She assured me that a small dose of Zoloft, an antidepressant medication, should take care of the issue.
I left the doctor’s office feeling relieved. The psychiatrist didn’t seem too concerned about Jamie’s behavior. She treated the situation with the same level of seriousness as that of a child with mild allergies who just needed a little allergy medication to control their symptoms.
Jamie began taking the Zoloft, and it didn’t take long for me to see that was all she had needed. It helped to calm her down, and she returned to her old self…at least for a while.
Jamie began worrying about things. Sometimes, they were just little insignificant things, but then they became more serious. When we talked, she would calm down, but eventually, she would return to them again and again. It seemed she couldn’t let these worrisome thoughts go.
Seeing that Jamie’s level of anxiety was increasing, the psychiatrist raised her Zoloft dosage, and again, this seemed to take care of the problem... for a while.
The anxiety would periodically return, and each time, the psychiatrist simply increased her Zoloft dosage. By the time Jamie turned 17, she was taking 250 mg. When I went to pick up the new prescription, our pharmacist pulled me aside and expressed his concerns. He told me that 250 mg of Zoloft was too high a dose for her.
The following day, I expressed my concerns to her psychiatrist, who, in response, switched Jamie from Zoloft to a low dose of Celexa, also an antidepressant medication.
It was about this time, Jamie started complaining about being tired. At first, it was only an occasional complaint, but I became worried when she started coming home from school too tired to do homework. She began going to bed around six and sleeping 12 to 13 hours every night. Our family doctor didn’t seem concerned and told me to let her sleep whenever she needed to.
Chapter 7 Living With Anxiety
In middle school, Jamie kept busy with drama club, orchestra, and soccer. But by the time she entered high school, her lack of energy prevented her from participating in extracurricular activities.
When Jamie turned sixteen, she began working a few hours a week at a local restaurant. The manager wanted to hire her as a food server or a hostess, but Jamie surprised her by choosing to be a dishwasher. She told me she chose this position to help keep her stress level down. Because she would be working in the back of the restaurant, primarily by herself, she could avoid all the hectic activities going on in the dining room.
Jamie didn’t have close friends now, even though she was well-liked; it just took too much out of her, pretending everything was okay while hiding her anxiety from others. During school lunches, she would choose to sit with a different group of students depending on where her stress level was on any particular day.
On difficult, stressful days, she sat with her quiet friends from the orchestra. On good days, she chose the energetic, lively kids she knew from drama club.
Then, there were days she sat with students from some of her classes that she barely knew. Because she didn't know them that well, she could avoid joining in on their conversations and sit quietly, eating her lunch.
Chapter 8 Second Opinion
From here, I use random names to identify doctors to protect their anonymity.
After the overmedication incident, I had lost confidence in Jamie’s psychiatrist and decided to seek a second opinion. Jamie was about to turn 18, which made her eligible to be seen by an adult psychiatrist.
When we had our first appointment with the new psychiatrist, Dr. Jackson, I was impressed; she was younger, soft-spoken, and showed a great deal of empathy for what Jamie had been going through.
After her assessment, Dr. Jackson decided Celexa was the appropriate medication for her to remain on since Jamie appeared to be managing well. I felt relieved when we left the office, confident that Jamie was in good hands.
Chapter 9 Starting College
The big day finally arrived! After graduating from high school, Jamie was heading off to college. Her goal was to earn a bachelor's degree, but I wasn’t too thrilled about the field she had chosen; it was in film. But of course, I couldn’t discourage her from following her dream of becoming the next Steven Spielberg?
I finally asked how she had come up with the idea to become a movie director, and she responded, “When I was little, I watched a cartoon, and when it was over, I thought to myself, ‘I could have made it better.’” After hearing that, I was 100% behind her career choice.
Everyone was urging me to send her to California, the movie-making capital of the world, but how could I? We lived in a small Midwestern town, and California was so far away.
After doing some research, we found a university two and a half hours away from where we lived that offers a bachelor’s degree in film. I could live with that, and because it was in a large metropolitan area, Jamie loved the idea of living in a big, bustling city. So off to college she went.
There were two occasions in Jamie’s life when I cried like a baby: one was when her dad missed her first day of school, and the second was the day I dropped her off at college. After giving her a big hug and leaving her at her dorm, I cried most of the two-and-a-half-hour drive home.
My sadness stemmed from Jim not being there to see what a wonderful young woman his daughter had grown up to be. From the first day she was born, he had always referred to her as his "Princess Jamie."
Chapter 10 Freshmen Year
In the beginning, Jamie did very well living away from home. She enjoyed her classes and liked all the instructors. Ironically, her student advisor was an older woman who shared that she, too, suffered from GAD and proved to be a great support person for her.
Knowing it would be overwhelming for Jamie to deal with the added stress of roommates, I arranged for her to have a private room. I even went the extra mile and secured a room on the top floor, where the older, more serious students lived.
This decision helped Jamie avoid the wild antics of the younger students on the lower floors, allowing her to get a good night's sleep. This private room would also provide a safe haven for her to go to whenever her anxiety flared up.
I felt satisfied that she was going to be okay and returned home, thinking everything was going great in our lives. However, these feelings were to be short-lived.
Chapter 11 Winter Break
I picked Jamie up from school for her first Christmas winter break. She had just finished her last exam, and as we drove out of town, we chatted away, looking forward to the holidays together.
Suddenly, seated next to me in the passenger seat, Jamie started complaining she couldn’t breathe. After several scary moments watching her struggle, I felt immense relief when she began breathing normally again and assured me she was okay.
Jamie described this frightening experience: “I felt as though I was breathing, yet at the same time, it felt like I was holding my breath and on the verge of passing out.” I was to learn later that what she experienced was a panic attack.
In the following days, Jamie’s anxiety quickly spun out of control. I was grateful she was home and could be seen by her psychiatrist. Jamie described the scary car-breathing incident to Dr. Jackson. To both our surprise, she didn’t seem concerned. She told Jamie that it was clear she was handling living away at college and doing well with her classes, suggesting that she couldn't have too much of a problem going on.
However, at the end of their meeting, Dr. Jackson switched her medication from Celexa to a drug called Prozac, another antidepressant, telling Jamie that it could take weeks for this drug to take full effect and to be patient.
After the holidays, Jamie returned to school, and I began receiving phone calls from her. Although we had always talked frequently while she was away at college, these calls were different. We spent most of the conversation discussing the troubling thoughts she was experiencing.
These conversations were usually about trivial matters that hardly warranted much thought, let alone her overreactions toward them. She was having increasingly frequent emotional meltdowns, struggling to control her thinking, and frustrated by her inability to calm herself down.
Most of the time, I simply listened and reassured her she wasn't going crazy, gently guiding her back to a place of reason until she could return to rational thinking.
Our phone calls usually lasted about half an hour and were reminiscent of the days in fourth grade when she would come home, obsessing over her small hands and stubby fingers in orchestra class.
As time went on, Jamie’s anxiety was getting significantly worse. She was now experiencing out-of-control meltdowns several times a week and struggling to keep up with her classes. Looking for help, she became a frequent visitor at the college’s counseling center.
The support she received from the counselors helped her to endure the waiting period for the medication prescribed by Dr. Jackson to take its full effect and provide relief from her constant feelings of anxiety.
It became apparent after weeks on Prozac that this medication was not helping. After Jamie contacted Dr. Jackson and described the symptoms, her psychiatrist switched her from Prozac to Cymbalta, another antidepressant, but also added Alprazolam (also known as Xanax), an anti-anxiety drug.
Chapter 12 More phone calls
As the days went by, the phone calls increased. What had been once a day began turning into two, even three times a day. Each time I answered the phone, I could hear the panic in Jamie’s voice.
Thankfully, our conversations usually helped her regain composure, but I felt helpless; all I could do was act as a sounding board for her to express the fears coming from her anxiety. I had to reach deep down inside myself to find the patience I needed, so I didn’t get overwhelmed with the exaggerated, distorted thinking her GAD was creating in her mind.
This was such an incredibly difficult time in our lives that it’s hard for me to put it into words. I didn’t understand what was happening to my daughter, but I knew her well enough to believe she was experiencing something terrifyingly beyond her control.
Weeks went by, and realizing that the recent change in medications, if they were going to work, should have kicked in by now.
Jamie contacted her psychiatrist again, who agreed to try another medication. This time, she replaced the Alprazolam with Buspirone HCL, which was another anti-anxiety medication.
Several more weeks passed, and still, no relief.
Jamie was now in an almost constant state of anxiety during her waking hours and had begun experiencing rapid heartbeats, hand tremors, shortness of breath, and profuse underarm sweating.
She started wearing absorbent pads in her underarms to soak up the sweat and became so self-conscious of the odor and underarm stains that she stopped raising her hand in class.
To make matters worse, Jamie was embarrassed by the terrible, ugly acne that had appeared all over her face, which the dermatologists were unable to help with.
Chapter 13 Navigating Life With An Anxiety Disorder
Jamie worried her classmates were noticing her hands frequently shook, and she had a deep fear that if people found out about her GAD, they wouldn’t want to be around her.
Because she suffered from unpredictable panic attacks, she found it harder and harder to connect with the other students or make plans to spend time with them outside of class.
Her private dorm room proved to be life-saving. It was the one place she could go without having to pretend, allowing her to let down her guard and cry as much as she needed without embarrassing herself in front of others.
When stress overwhelmed her at school, the one place she could escape to was the nearest public bathroom stall. Even the fear of classmates questioning why she had a private room on the fourth floor and not knowing what to say without lying caused her stress.
She fretted about anything and everything that she perceived as having even a remote chance of escalating her anxiety, leading to another panic attack.
By the end of most days, Jamie was left completely spent from the energy it took living with her anxiety disorder. Many mornings, she would roll out of bed and drink a large cup of coffee to help make it to class. Afterward, return to her dorm, fall back into bed, and sleep for hours.
Not even strong coffee could counteract the exhaustion her GAD was creating.
Chapter 14 ‘The Worries’
After weeks of being on the Buspirone HCL and still not feeling any relief, Jamie decided to check in with the college’s psychiatrist, Dr. white. This doctor really took the time to listen to Jamie as she shared her list of symptoms she had been living with. After a full evaluation, Dr. White recommended stopping the Buspirone and replacing it with Lorazepam, another anti-anxiety medication.
It was heartbreaking every time Jamie shared with me what she was going through. She told me she worried about worrying, explaining that after each panic attack ended, she would immediately begin worrying about the next one and whether it would be the one she would not be able to recover from.
Chapter 15 More Drugs
Looking for help, Jamie returned to the college counseling center and found Dr. White had suddenly retired. She was referred to Dr. Richards, who, after looking over her records, prescribed Lexapro, an antidepressant used to treat anxiety and depression, in place of Lorazepam. When this medication failed, Dr. Richards prescribed Gabapentin, an anti-epileptic drug, and then Clonazepam, an anti-convulsive medication.
As the months went by, none of these medications brought the relief Jamie was hoping for or had even helped to lessen her anxiety symptoms.
Now, to let my reader know, there are consequences every time Jamie experiences a drug change. There would be a period of withdrawal symptoms to weather through each time, and if she was lucky, it would be mild symptoms, or they could be as unpleasant as flu symptoms.
Jamie’s anxiety would become so unpredictable during prescription changes that the flare-ups sometimes left her feeling so emotionally confused that she couldn’t trust her own feelings or perceptions.
Chapter 16 Yoga?
Jamie came home for summer break and returned to Dr. Jackson, telling her the medications Dr. Richards had prescribed had not helped.
Dr. Jackson showed very little empathy towards Jamie this time and simply told her she needed to do yoga, adding that some of her problem was her unwillingness to work harder at controlling her stress.
Desperate to try anything, Jamie made an appointment at a local rehabilitation center and received a yoga lesson, but found she couldn’t do it. Her anxiety prevented her from staying calm and centered long enough to concentrate and take in the information needed to learn proper yoga poses.
Later I would learn that during anxiety flare-ups, people with GAD struggle with short-term memory, difficulty concentrating, and retaining information. Today, Jamie refers to this as ‘brain fog.’
I admit, as time went on and the more I learned about GAD, how regretful I became, out of ignorance, over some of the ways I handled Jamie in the early stages of her disorder.
Pressure from her doctor and me to take up yoga only created more anguish in Jamie. She began blaming herself it was her fault that she had GAD. The message she heard from Dr. Jackson was: ‘She should be able to control her anxiety if she wants to.’
As Jamie and I say today, ‘When we know better, we do better,’ but at this point in the story, I was clueless about what we were dealing with. It was bigger than the two of us and apparently bigger than the doctors she had been seeing.
She saw Dr. Jackson one more time before returning to school. The session only lasted a short time, during which Jamie again conveyed to her the fear of nothing working to ease her anxiety. At the end of the visit, after nearly two years of treating Jamie, this doctor simply looked at her and said, “I don’t know what else you expect me to do?” and indicated their meeting was over.
Chapter 17 A New Approach
Jamie was plagued with thoughts that she projected out into her future with what we call the ‘What Ifs.’ For example, what if her GAD prevented her from getting an internship or a job? What if she was forced to leave college? And her biggest fear, what if there was no cure for her condition?
As a mother, I was desperate. Having a mental health degree myself and having been a drug and alcohol abuse counselor prior to my marriage, I was sure the medical field should have more to offer Jamie than what her psychiatrists had.
I began researching Generalized Anxiety Disorders and found that experts considered cognitive-behavioral therapy a viable treatment for GAD. I sought out a psychologist specializing in cognitive therapy.
At our first meeting, she told my daughter to “Put her troubles in a bubble and send them up into the air.” I knew right away this woman had no idea what she was dealing with. Also, this was the first professional to broach the subject that Jamie was probably suffering from a childhood trauma that was causing her anxiety, called PTSD, post-traumatic stress disorder.
The idea of PTSD was scary for me as a mother. Was I the blame for Jamie’s problems for something I had let happen to my daughter while growing up?
The psychologist sent a questionnaire home for Jamie to fill out. This questionnaire was so in-depth and complex that anyone filling it out and answering it truthfully could not deny or hide any signs of deep emotional conflict rooted in their psyche.
After the psychologist received and reviewed the questionnaire, to my relief, she declared, ‘Jamie did not have PTSD; she just suffers from anxiety.’ But wait, was this something I should have been relieved about? If we could have identified a past incident buried in her memory, could it have helped her?
Unfortunately, the only help we received from this professional was confirming a diagnosis we already knew.
But I still needed answers as to what was wrong with my daughter.
Chapter 18 The Worst Mistake
When summer break finally came, I made the worst decision I could’ve ever made. I took Jamie off all the drugs. My attitude was, “If they weren’t working, get her off of them.” We then headed to the beach for a much-needed vacation.
Jamie was void of all emotions during the entire week and spent most of the days sitting around doing absolutely nothing, even though we were next to the beautiful ocean having fantastic weather. I genuinely believed that getting away and having a change of scenery would help.
ALERT TO ALL-Never abruptly stop medication without consulting a doctor or pharmacist.
I didn’t know at the time, but some of Jamie’s behavior was from thoughts of doom and gloom, believing she would never be happy again, and some were from drug withdrawal symptoms.
She complained of having electric shock sensations in her head that she could only describe as: “Like when you begin to fall asleep and jerk yourself back awake, except I wasn’t asleep, and they're happening inside my head, and it's only my eyes that jerk back and forth.”
Years later, I learned that withdrawal from antidepressants and anti-anxiety medication can involve symptoms such as anxiety, depression, mood swings, fatigue, flu-like symptoms, headaches, nausea, tremors, trouble sleeping, and electric shock sensations Jamie experienced as ‘head zap.’
When Jamie returned home, we hadn’t yet lined up another psychiatrist, so she had no other choice but to return to Dr. Jackson.
Jamie described her relentless anxiety attacks. Dr. Jackson sat and listened, then asked if she thought she could have a bipolar condition (also can be called manic depression, in which the person vacillates between extreme uncontrollable high and low moods).
Jamie was confused and couldn't even answer; she had no idea what she was suffering from. Dr. Jackson just shrugged her shoulders, making no further attempt to continue the discussion, and proceeded to prescribe Lexapro for her.
Jamie tried to tell her she had been on Lexapro before and that it hadn’t helped. Dr. Jackson explained that sometimes, when a drug stops working, you can cycle through other prescriptions and come back around to find that it will work the second time.
This made little sense to us since Lexapro hadn’t worked the first time, let alone stopped working, but Dr. Jackson gave no other options, so Jamie went back on the Lexapro.
Up until now, the psychiatrists Jamie had met with seemed not to have any answers other than to give her drugs. When the drugs didn’t work, Dr. Jackson blamed her for not managing her stress effectively, convincing Jamie that it was within her power to stop the panic attacks. As a result, Jamie began developing unhealthy thinking and behavior patterns, pressuring herself to get on top of her GAD.
Jamie began developing an extreme case of perfectionism. She believed if she didn’t do anything wrong, she should be able to avoid having the next panic attack.
She began pressuring herself to keep everything running smoothly in her life. If she perceived that she had messed up, it was hard for her to let go of the feeling that she had done something wrong. She would replay the situation in her mind over and over again, imagining different scenarios, such as: ‘If I had only done this instead of that, I could have prevented a panic attack.’ She also became obsessed with over-preparing for upcoming events to avoid any potential mishap that might trigger her anxiety.
Chapter 19 Another Opinion
In the fall, Jamie was able to obtain a referral to see Dr. Blaine, a well-respected psychiatrist. After her first visit with him, she called me from the parking lot, crying. I thought something terrible had gone wrong, but no, Jamie was crying with a deep sense of relief because this doctor had said he thought he could help her.
Dr. Blaine continued to prescribe Lexapro but added Gabapentin, an anti-epileptic drug used for seizures.
Because of the weeks it takes for a drug to take its full effect, it meant long weeks filled with anticipation, waiting to see if this would be the one to ease Jamie’s suffering.
It was agonizing to watch her disappointment and loss of hope each time the drugs failed. But the thought of giving up was not in her nature.
Chapter 20 2nd Year At College
Jamie returned to school. She worked hard and received good grades. Looking back, I don’t know how she did it. Day after day, meltdown after meltdown continued to plague her.
The daily phone calls to process her latest fears could now easily last forty-five minutes to an hour or longer, taking up a large part of our day. Even if she could quell one fear, another one would be waiting to emerge.
She was in an endless cycle, exhausting herself keeping up with her classes, and obsessively searching for ways to avoid the next panic attack.
If, for some reason, I was unavailable or needed a break myself, Jamie made good use of the college’s counseling center. She never hesitated to walk in asking for help.
Adding to her grief, some of the counselors had begun pushing their own theories. They believed that someone who suffered from the severe anxiety Jamie was experiencing had to be caused by avoiding some traumatic incident from their past. They kept insisting that if she opened up and dealt with it, it would probably ease her panic attacks.
Chapter 21 Making The Most Of It
There were brief periods of time when Jamie felt more like herself and could actually get a chance to enjoy college life. These were times when she was fully engaged in an activity that kept her from dwelling on scary thoughts. She created things to look forward to, no matter how small, like a favorite meal or a good movie.
One thing I was grateful for was Jamie’s love for computer games. The dorm had a great computer lab, which she used frequently, especially on weekends, providing a bit of downtime.
She enjoyed playing the live online interactive games with other gamers, primarily because they communicated through text. Since everything is happening online, Jamie didn’t have to pretend or put up a front while playing; she could be herself, sitting all alone at the computer and, if need be, let herself cry, knowing the other players she was texting couldn’t see or hear her.
I can’t tell you how much our lives had changed. It seemed we were engaged in fighting an invisible monster that only Jamie and I knew was there.
If you couldn’t see it on an X-ray, a blood test, or as obvious as a broken bone, some professionals she was seeing couldn’t believe or understand the severity with which Jamie suffered from GAD. They saw her successful in her studies and living independently away from home. From their perspective, it couldn’t be all that bad.
I don’t believe they thought she was exaggerating her symptoms; I think they just didn’t know how to help her.
Chapter 22
When the Lexapro and Gabapentin Dr. Blaine prescribed did little to ease Jamie’s symptoms, he then prescribed Prozac for her depression and Xanax for the panic attacks.
Both of these drugs had been tried before by Dr. Jackson, but Dr. Blaine gave the same explanation we had heard before: Sometimes you can cycle through different drugs, and on the second time around, find they work.
Although Jamie had her doubts, she followed Dr. Blaine’s instructions.
Jamie had now convinced herself she definitely suffers from PTSD from counselors, pushing their theory that a past event was causing her GAD. She became fixated on trying to remember what traumatic event could have been responsible for her illness.
She peppered me with questions about any and all negative incidents I could remember, firmly believing, ‘if she could just remember,’ it would cure her.
I was desperate to help, so I relayed every negative experience I could remember, holding nothing back; no matter how uncomfortable it was for me or any of my past behavior.
Out of all the memories I shared with her, Jamie also could remembered them, so none of them fit the trauma criteria she was looking for.
There was nothing I could do to stop this obsession. Even when I reminded Jamie of the in-depth questionnaire the cognitive behavior psychologist had given her, ruling out PTSD, it didn’t make any difference.
Chapter 23 Junior Year
Despite everything going on, Jamie returned to college for her Junior year. I questioned whether she was up to it, but she told me there wouldn’t be any reason to keep going if she dropped out of school now, believing her life would be over.
We still had our daily phone calls, and Jamie continued to seek support from the school’s counselors, but now suicidal thoughts were beginning to creep into her mind. However, she wasn’t sharing these thoughts with anyone.
Years later, I discovered she had written a suicide note to me once, but decided she wasn’t ready to die and tore it up.
While writing this story, Jamie told me there had been many times when she thought her life was hanging by a thread. This is her description of one of those times:
One day, while I was sitting in class, I had reached the end of the rope dealing with my anxiety. Feeling like I couldn’t handle one more panic attack, it suddenly dawned on me that I had, within me, the power to stop it; I could kill myself. When this thought came to me, I felt a sudden sense of calmness wash over me. The idea of suicide was so real that at that exact moment, a tremendous feeling of fear shot through me. After class, I went straight to the counseling office, walked in, and told the first person I saw that I wanted to kill myself.
The office workers rushed around and got me into one of the counselors, who was able to calm me down. I gave them my assurance that I would not commit suicide before they allowed me to leave.
Years later, when I told Mom this story, she asked what kept me from doing it. I answered, “If I take my own life, I will never know how my story is supposed to end, so I decided to hang in there and keep going.”
As a mother, discovering how close I came to losing my daughter was traumatizing. I knew she was suffering tremendously, but never realized how her despair could take her to such a dark place. Looking back, I realize now that both the psychiatrists and I were only seeing the tip of the iceberg of that suffering.
I will always be eternally grateful to the staff who happened to be on duty that day. If Jamie had called me with suicidal thoughts, I’m sure I would have handled it differently, probably insisting she come home; instead, the counselors were able to instill in her the will to keep fighting, which was, by far, a much better choice than what mine would’ve been.
Chapter 24 The Physical Toll
That spring, Jamie’s physical symptoms escalated. She was familiar with profuse sweating, fatigue, problems breathing during anxiety attacks, shaky hands, upset stomach from all the drug changes, and now hair loss. But the scariest one was when her heart rate started going off the chart, sometimes as high as 140 beats a minute, accompanied by lightheadedness whenever she stood up.
She headed to the hospital and found herself hooked up to a heart monitor. The doctor told her that an anxiety disorder could be masking a heart condition.
Surprisingly, Jamie said a heart condition would be a welcome diagnosis. To her, a heart problem sounded like an easier fix compared to her track record of treating her GAD.
The heart monitor and an ultrasound revealed nothing abnormal. But there was one more test—the tilt table test. This test revealed a diagnosis of POTS, postural orthostatic tachycardia syndrome. The simple explanation we received was that Jamie’s heart has trouble bringing blood up from the lower part of her body, causing lightheadedness whenever she stands up.
At the same time as the POTS diagnosis, a blood test revealed Jamie had a dangerously high level of liver enzymes, equal to that of a chronically heavy drinker. Since Jamie doesn’t drink, the cardiologist determined it was the drugs prescribed by her psychiatrist causing the liver problem.
When Dr. B. was notified of her condition, he abruptly took her off her medications, which, of course, triggered a whole host of severe withdrawal symptoms.
It was disturbing to learn that the drugs given to Jamie could have caused permanent liver damage if not discovered in time. It made me question what other dangers these drugs were capable of, and should she be monitored more closely?
So here we are. Okay, I thought, withdraw Jamie from the medications to take care of the liver issue and the non-threatening heart condition she can learn to live with, except the doctor never told Jamie what to do living with POTS.
So now she lives with her heart beating an average of 140+ beats a minute at times, suffers from lightheadedness, daily panic attacks, and all the other symptoms she developed that go along with having GAD (generalized anxiety disorder).
Chapter 25 The Fifth Psychiatrist
The cardiologist suggested Jamie be seen by the hospital's psychiatrist, Dr. Adams. At their first meeting, this doctor prescribed the antidepressant Lexapro but added a beta blocker, Propranolol, to help with the racing heart symptoms.
Jamie continued to see Dr. Adams until this happened; During one of their sessions, Jamie was attempting to convey to this doctor how bad her anxiety had gotten. Out of the blue, Dr. Adams leaned forward, pointed a finger in her face, and said in a mean, harsh voice, “See, it’s your thinking that’s causing your problems.” Jamie was shocked and, needless to say, deeply hurt by her reaction.
When she relayed this incident to me, it was one of the lowest points in my life. This doctor, at one of the most highly respected hospitals in the country, had not only failed to help my daughter, but was another professional telling Jamie her anxiety was her fault.
Jamie never returned to Dr. Adams.
Side note: I know Jamie can be very frustrating to talk with during one of her anxiety attacks. She struggles to think rationally; her mind races, and sometimes she can run through her scary "what if" scenarios faster than I can keep up with. Often, before I can finish a sentence, her mind has already jumped ahead to the next fear that has just popped into her head, often changing the subject mid-sentence.
Anyone who has had experience trying to reason with a person who is in the middle of an anxiety episode can probably identify with this behavior.
I cannot blame Dr. Adams for getting frustrated with Jamie and cutting her off; she’s only human. But what surprised me was the manner in which she had said those accusatory words to her. Surely, this doctor knows that people with mental disorders didn’t ask to have them.
Today, I have a better understanding of why Jamie constantly struggles with anxiety and often has intense reactions, causing her to lose control of her emotions. Later in my story, you'll also learn more about what is happening in Jamie’s brain when she is experiencing an anxiety attack.
Chapter 26 Continuing To Seek Help
It is now at the end of Jamie’s Junior year. Seeing her anxiety disorder history and her POTS condition, her heart doctor told her to go home, take the summer off, and REST. So home she came, exhausted, discouraged, and, of course, full of anxiety. At 21 years old, it has now been 8 years since we began this journey.
After returning home, Jamie decided to enroll in a summer class at the local college campus, not only to beef up her credits to stay on track to finish school in four years, but also to help occupy her mind. She also took this opportunity to check in with the school counselor.
This woman was wonderful. She worked with Jamie on the childhood trauma issue that had been plaguing her. When talk therapy couldn’t raise any memories, the counselor decided to try light therapy, a type of treatment developed to help returning veterans suffering from PTSD (post-traumatic stress disorder). This therapy works to enhance communication between the brain’s regions responsible for emotions.
During a light session, the person is asked questions and encouraged to discuss deeply rooted, disturbing incidents buried in their memories. Jamie was so desperate to get well that she quickly spilled out anything and everything she could remember that had ever been an unpleasant experience.
The counselor was so impressed with Jamie’s recall ability that she was confident in stating, “In my professional opinion, childhood trauma did not cause Jamie’s anxiety, and she appears to have no repressed memories.”
Once again, we were told that she just suffers from anxiety. However, Jamie still remained convinced that childhood trauma was the source of her anxiety. It was hard to reason with her when her body and mind were constantly in a state of turmoil.
Even when I reminded her again of the questionnaire she had filled out years ago with the cognitive therapist, it didn't make a difference.
She continued to 'witch hunt,' constantly looking for the past incident that could account for her GAD, that previous counselors had insisted ‘must lie in her childhood.’
It was a scary world going on in her head, and frightening for me to watch her spiral down into a state of hopelessness of ever finding answers.
Chapter 27 Taking A Break
After completing her fourth year at college, Jamie was supposed to graduate in the spring, but found she was short a few credits and needed to do an internship to fulfill those requirements.
I told her to come home, take the summer off to rest and regroup before tackling the pressures of pursuing an internship. So home she came.
During that summer, whenever the weather was nice, we planned day trips to get out and enjoy ourselves. However, time and time again, we would get in the car and be on our way, only to have to turn around because Jamie’s anxiety would flare up.
I was beside myself, seeing the sad, empty look in my daughter's eyes. She was so far away from the happy, energetic kid I had known in the past.
As a mother, I was so fearful for her, but I never wanted to convey this to Jamie. I didn’t want her to worry any more than she already did about what was going to happen to her.
I continually assured her that we would find the answers to her generalized anxiety disorder (GAD). But I was starting to have my own doubts.
Chapter 28 Back On Her Own
In the fall, I knew it was time for Jamie to return to her life. Together, we found her an apartment near the college. Her game plan was to get a part-time job, complete an internship, and earn her diploma.
Jamie was able to get a low-stress job working a few hours a week at the college’s disability office. She also lined up a new general practitioner, Dr. Spragg.
After reviewing her history, Dr. Spragg was the first doctor who admitted the medical field had failed Jamie and that more should have been done to help ease her suffering. She prescribed Atarax, an antihistamine product developed for anxiety, along with Duloxetine, used for depression and anxiety, optimistic that these drugs would help.
When this drug combination failed, Dr. Spragg prescribed Loestrin, a birth control pill to help even out her emotions, and put her back on a beta blocker, Propranolol, for the rapid heartbeats Jamie still experiences.
When these drugs failed, Dr. Spragg, who had started out being so supportive, now did a complete turnaround, sending the message Jamie had heard before, “I don’t know what else you expect me to do?”
She went to this doctor in tears, asking for help, and when the drugs failed, she was once more left on her own without any answers.
I was angry and frustrated every time Jamie told me what was happening behind closed doors, and the treatment she received from some of the doctors she saw. This was a repeat of what happened with Dr. Adams, who had gotten mean, blaming her ‘thinking’ for her GAD, or Dr. Jackson, who told her it was her unwillingness to work harder at controlling her anxiety was the problem.
Now you might be asking, is Jamie difficult to get along with, maybe a little spoiled, or obstinate because she is an only child? Well, let me set you straight. Jamie is far from perfect, but she is also one of the most caring people you will ever meet.This is not only my opinion. It's a common sentiment shared by nearly everyone who knows her, to hear people often say, "She’s so sweet." Even though Jamie never knew her father, she has his same easygoing personality and pleasant disposition.
I don’t know what happened in meetings that would cause these doctors to turn on her and lose their patience. It seemed to me they surely must have known their uncaring, mean, or sarcastic behavior would discourage her from returning to them. I just couldn’t understand why they acted this way.
What do we do? Where do we turn? I could see Jamie was nearing a breaking point. Her symptoms had become so debilitating that everyday activities such as doing laundry, grocery shopping, and even meal preparation had become major obstacles for her. The toll her anxiety was taking on her had become too much.
Chapter 29 Bringing Her Home
Her job contract had ended, and seeing her struggling, I finally told her to close up her apartment and come home. If she was heading for a complete breakdown, I wanted her home with me.
Jamie came home and spent most of her days lying around on the couch. She looked emotionally drained, apathetic, and appeared to be giving up. I encouraged her not to lose hope and to make an appointment with our family doctor, Dr. Stephens.
During her appointment, Dr. Stephens reviewed all the medications Jamie had tried. She decided to prescribe Metoprolol ER to lower her blood pressure and reintroduce Clonazepam, the anti-epileptic seizure medication she had been on before.
Nothing was working. I felt helpless. Again, I had to ask, What do we do, and where do we turn?
Little did I know that an answer to my questions was about to come our way and change the whole ballgame.
Part 2
Chapter 30 Hope
Jamie is now 23, and still living at home with me.
One morning, I was watching a talk show, and a doctor from an Integrated Medicine program at a highly respected hospital happened to be the guest speaker. I don’t recall exactly what he said that made me think he could help Jamie. I don’t even think he mentioned anxiety. What he did say was that their department was all about integrating wellness into every patient.
I asked Jamie if she thought this program was worth looking into. She gave a resounding "yes," willing to try anything, even if it was a long shot.
The following week, we found ourselves in the office of Dr. Baker, an internal specialist, at the Integrated Medicine department. She listened as Jamie recounted the long list of symptoms she had been living with.
What stood out most from the conversation, however, was when Jamie mentioned her Aunt Lois, from her father's side of the family, who had been institutionalized in a mental hospital in the 1950s.
Dr. Baker immediately seized upon this crucial information. She theorized that it was quite possible Jamie had inherited mutated genes that could be the culprit for her GAD. I’m sitting there, hearing this new information, stunned. Could it be the explanation we had been searching for?
Dr. Baker ordered tests, and sure enough, the tests came back confirming her suspicions. Jamie had inherited three mutated genes: a double copy of an MTFHR gene, one from her father and one from me, and a third one. We were told that the combination of these three mutated genes often manifests itself in anxiety disorders.
We finally had an answer to Jamie’s condition! Dr. Baker prescribed Sertraline, also known as Zoloft, which, if you remember, was the first medication Jamie was prescribed years ago when she was first diagnosed with GAD.
Dr. Baker also prescribed a 5-MTHF, a folate supplement, and vitamin B’s to help compensate for the body’s defects caused by her particular mutated genes.
Jamie also explored the alternative treatments offered by the Department of Integrated Medicine, experiencing hypnosis, acupuncture, and meditation techniques.
Now, you may think we have come to the end of our journey, but unbeknown to us, we were far from it. It wasn't long after Jamie began following Dr. Baker's recommendations that it became clear the relief she was hoping for wasn't happening.
There were times when Jamie seemed a little better, but then the ‘anxiety dragon’ would lift its head, and the panic attacks returned in full force.
One morning, shortly after beginning the regimen Dr. Baker had prescribed, Jamie woke up in a panic. The entire right side of her body was numb and tingling. We rushed to the emergency room.
After running tests and finding nothing wrong, the medical staff determined it was a reaction to the high levels of Vitamin B she had been taking.
Jamie stopped taking the vitamins, and the numbness and tingling completely disappeared within a couple of days.
It appeared that Dr. Baker didn’t have all the answers after all.
The most important takeaway from Jamie’s visit to Integrated Medicine was the realization that her Generalized Anxiety Disorder is not her fault. It was caused by an unlucky draw of the mutated genes. AND FINALLY, she was able to let go of her obsession with the childhood trauma theory, which she had long believed was responsible for her GAD, that had tormented her for years.
Even though the numbness Jamie experienced that sent us to the emergency room had resolved itself, I still had concerns. Could she be developing neurological issues along with her GAD? I decided to have Jamie evaluated by a neurologist.
The neurologist was kind to Jamie. After reviewing her test results, he had no answers to explain her symptoms. He was very compassionate though, and wished her well, telling her not to give up.
After the failure of integrated medicine, we were back at square one. I was desperate, believing time was running out for my daughter.
Chapter 31 A New Approach
During one of our visits to Integrated Medicine, Dr. Baker pointed out the fact that not only had Jamie inherited mutated genes, but I also had one of these mutated MTFHR genes associated with anxiety.
When I heard this, I realized that stress had always been a factor in my life. Looking back, I can acknowledge that during my young adult years, I unfortunately made some poor life choices.
I realized that I had avoided stressful situations, such as leaving jobs or ending relationships, to manage my anxiety, rather than confronting and resolving the issues within them.
I had always assumed my stress levels were normal compared to what other people experienced, but now I questioned that notion and found myself curious to learn more about my own relationship with anxiety.
Dr. Baker had recommended a book she thought might provide more insight into the mind-body connection, believing it may help Jamie and me to understand Generalized Anxiety Disorders better.
After returning home, I began reading the book. It explained in detail how to get the body functioning at optimal levels. It outlined a comprehensive treatment plan that included healthy eating, avoiding food sensitivities, taking supplements, and guidelines for living a healthy lifestyle.
I began to wonder, if Jamie did everything to optimize her health, could it help with her GAD symptoms? At the end of the book, there was a biography of the doctor who had written it, along with the name of his program, called Functional Medicine.
It just so happened that the location of this program was in a city nearby to where we lived.
The following week, Jamie and I met with Dr. Parker at Functional Medicine. He was wonderful. After reviewing her history, he was the first person who explained to us what was going on in her brain: Jamie has a barrier that prevents her from methylating vitamin B, an essential vitamin for brain health. Her brain also absorbs serotonin too quickly, the happy hormone responsible for stabilizing our moods.
He told us that Jamie’s body cannot regulate the chemicals in her brain like it should. Consequently, her brain will simultaneously release surges of adrenaline, hormones, and insulin that overwhelm her body, triggering a "fight or flight" response, resulting in a panic attack.
Dr. Parker gave an excellent example of this brain function:
A person driving their car down the street approaches an intersection, and for a split second, they are distracted and look away. When they look back, they immediately realize they are about to run into a car that has suddenly stopped in front of them and slams on their brakes. That small jolt felt when someone encounters a sudden, unexpected emergency situation is a surge of brain chemicals. When the brain is working correctly, a person can pause, gather their thoughts, calm themselves, and continue driving, grateful they have avoided an accident.
For Jamie, she cannot calm herself down; for her, it’s a waiting game. She will remain in a heightened state of stress, possibly escalating into anxiety, until her brain chemicals even out. For her, this process can last anywhere from a short time to hours or even days.
Also, Jamie’s panic attacks can occur at any moment, with or without a warning or a cause. This condition is known as panic disorder (PD). Dr. Parker further explained that a panic attack can use as much energy as running a race. When it's over, the person is left exhausted.
Until now, there has not been a drug, counseling, or therapy session that has helped Jamie. However, having an explanation of her condition, rather than blame or apathy, can go a long way when she is at the mercy of the unpredictable nature of her brain’s chemical processes.
Chapter 32 The Functional Medicine Program
Jamie and I both came away with a renewed hope that we were going to find the answers to ease her symptoms.
Functional Medicine introduced a new approach to Jamie’s condition: FOOD. After extensive metabolic testing, it was determined that Jamie’s poor diet needed improvement. In addition, nutritional supplements were also recommended to help optimize her body’s functioning ability.
We were told that most of the neurons the brain needs for healthy brain function are manufactured in the digestive tract. Doctors refer to this as your ‘second brain,’ incapable of thought as we know it, but still communicates back and forth with our thinking ‘big’ brain.
Dr. Parker gave the example of this brain-gut connection, scientists call the Enteric Nervous System or ENS:
If you have ever acted on a ‘gut reaction’ or had ‘butterflies in your stomach,’ it’s your second brain talking to your big brain.
Chapter 33 Why A Healthy Diet?
It was explained to us that Dopamine, the neurotransmitter responsible for the feeling of pleasure, is made in our brain, but 95% of the body’s Serotonin, the happy hormone, is found in the digestive tract, along with 100 million neurons filled with essential neurotransmitters. These are the body’s messaging transmitters that determine our mental state.
A healthy diet is essential for the optimal performance of the neurons responsible for balancing both Dopamine and Serotonin, which Is Crucial for good mental health. A poor diet loaded with junk food and refined sugar is not very helpful in this process. After receiving this information, I was surprised that the psychiatrists had never asked Jamie about her diet.
This is just a tiny part of everything the digestive system is responsible for, but our focus is mainly on how Jamie’s diet could significantly impact her GAD symptoms.
This approach made a lot of sense to try since Jamie had never really eaten what I would call a healthy diet. Growing up, it was a constant battle to get her to eat vegetables, and at college, she lived on a diet of sandwiches, fries, and processed foods.
Functional medicine taught us that processed, heavily sweetened (including artificial sweeteners), high-saturated fat foods, and high-calorie snack foods contain harmful, unnatural chemical ingredients. If you already have a chemical imbalance, it is even more advantageous to avoid the harmful substances found in these unhealthy food choices.
They refer to a healthy diet as ‘clean eating’ because it avoids foods known for high levels of pesticides, such as berries, apples, leafy greens, tomatoes, celery, white potatoes, peppers, and foods containing nitrates, such as lunch meats.
To avoid pesticides, we were instructed to only purchase organically grown foods and grass-fed organic beef and dairy.
The goal was to give Jamie’s body and brain the best opportunity for optimal functioning in the hope of helping her manage her GAD.
Chapter 34 Supplements
This is the list of supplements the pharmacist formulated for Jamie's daily use, based on her test results. And yes, they were expensive:
B12 Folate-to address the MTFHR mutation
Ketoconazole shampoo for hair loss
Lavela WS-Lavender pill to aid in sleep
Progesterone micronized-hormone replacement therapy
Spironolactone-treats high blood pressure
Vitamin D3-address low vitamin D3 levels
Probiotics-for building healthy stomach enzymes
Trava Cor-to improve mood and reduce stress
Focus DL-for focus and cognition
Calm CP for sleep and management of blood sugar
Adre Cor with Sam e-for mood support and fatigue
After returning home with Jamie’s bag of supplements, we headed to an organic grocery store. Of course, we were not on our own; we had been given a strict, or should I say, a restricted dietary guidelines to follow.
We bought everything fresh. For protein, only lean meat and selected fish, prepared baked or broiled, and eggs were allowed. No legumes or dairy products, but nut milk, raw unsalted nuts, and seeds were permitted.
All leafy greens and vegetables were allowed except for starchy vegetables such as beets and white potatoes. The only fruits included in her diet were berries and kiwi, and absolutely no wheat, oats, or rice, but Jamie could eat quinoa as a substitute for these grains.
Beverages were limited to water and or decaf green tea, with no sugar or sweeteners. For condiments and flavoring food, only olive oil, vinegar, Dijon mustard, herbs, and spices were to be used.
This was the worst for Jamie. A typical meal might include a baked chicken breast, quinoa, and broccoli. In the beginning, she actually gagged while choking down vegetables, but persevered, desperate to try anything if there was even the slightest chance it would bring her relief.
I supported her by going on the diet along with her, but I only lasted three months. Jamie, on the other hand, hung in there for six months.
It was not easy for her during those six months. While on this diet, she had some of the worst meltdown days yet. One day, Jamie was in such a bad place that we headed to the nearest emergency room.
It was obvious she had reached a breaking point and had exhausted all her coping abilities. I cannot even imagine what she must have been experiencing that day to request to be taken to the hospital.
Once we arrived at the hospital and the staff assessed her, they found she was not suicidal and saw no other reason to keep her, sending us away.
Thankfully, by the time we returned home, Jamie had begun to calm down, but was exhausted. She went to bed and slept sixteen hours straight through to the following morning.
The next day, Jamie reflected on the events of the previous day. The best way she could describe it was, “It felt like electric stress was penetrating every cell in my body, and my whole body was going to collapse in on itself. I thought, ‘This is it, I’m going to die.’”
Continuing on, Jamie was now experiencing constant hunger while still struggling on the strict Functional Medicine diet. She was unable to maintain her weight, falling several pounds below the normal range recommended for her height. Even though her calorie intake was not limited, she couldn’t shake the feeling of not getting enough to eat, no matter how much food she consumed.
When we returned to Functional Medicine, it was clear that the diet plan and supplements had made little to no difference in Jamie’s symptoms.
After six months in the program, Dr. Parker informed us that if their program was going to work, it should have shown results by now. He mentioned that the program was effective for approximately 80% of the patients who tried it. Apparently, Jamie fell into the 20% for whom it did not work. Dr. Parker noted that Jamie appeared to be in good physical health and was sorry he had no other suggestions for further treatment.
I’m still glad we tried the diet, and Jamie now understands the importance of a healthy diet. To this day, she has stuck to many of the guidelines she learned for healthy eating, with one big exception: she has added healthy grains back into her diet that were forbidden on the Functional Medicine diet, and when she occasionally indulges in snack foods, she does so in moderation.
One symptom she still continues to struggle with since going off the strict Functional Medicine diet is her insatiable appetite. Even today, there are times when, no matter how much she eats, she feels like she can’t get enough food to feel full. On those days, she grazes continuously, usually craving high-carbohydrate foods like pizza and pasta. We don’t understand this behavior, and even though she consumes more calories on these ‘craving’ days, her weight hasn’t changed that much.
Chapter 35 Finishing Her Degree
Despite her struggles with anxiety, Jamie moved back into her apartment, successfully secured an internship, and finally graduated with a Bachelor's degree. However, regrettably, she found that she lacked the necessary skills to secure employment in the film industry. At every interview, she was told she needed more experience.
To beef up her resume, Jamie enrolled in digital film editing classes at a nearby technical college. She did well in her classes and was able to network with one of the instructors, who referred her to the head of a film department at a large hospital.
After interviewing for a job, Jamie was hired as a contract worker for the position of a digital film editor. This was a red-letter day for her. At 26, it meant she was financially independent for the first time in her life.
The benefits of this job included a good salary and flexible hours. Jamie could choose what days of the week she would work, which meant she could work her schedule around her anxiety.
Jamie worked three days a week, taking every other day off to rest and regroup. This was an absolute must because her anxiety was just as difficult living with as it had been during her college years.
Jamie’s anxiety significantly impacted her daily life, making it challenging to balance her job and responsibilities, resulting in her having very little time for social or enjoyable activities outside of work.
Working hard to maintain a facade of normalcy at work, Jamie was still fearful that if others found out about her GAD, they would think differently of her. During stressful moments, she made a habit of carrying a coffee cup around with her to conceal her shaky hands.
To relieve stress at work, she often sought the privacy of a bathroom stall in the employee’s restroom. During these times, she might call me for encouragement or cry quietly to herself, releasing the pent-up stress she was feeling. But Jamie enjoyed the people she worked with, and over time, her employer added more responsibilities to her job description, giving her a sense of achievement.
Because they had not been helpful, Jamie decided to go off all medications. Instead, she turned to exercise after reading articles that proclaimed the benefits of aerobic activity for reducing stress. She even gave yoga another try. Her POTS symptoms, however, proved too much to overcome, leading to frustration with these attempts. Each time she attempted to engage in any physical activity, her anxiety would spike along with increased rapid heartbeats.
Feeling more defeated than ever, Jamie returned to the Integrated Wellness Center and tried some of their holistic techniques, such as Tapping (a therapy in which a person taps different body parts to manage emotions) and revisited acupuncture and hypnosis. Nothing was working.
Chapter 36 Back To Square One, Again
Jamie began reading everything she could on her condition, from books used by therapists to treat anxiety in their patients to books on brain functions. She also tried various healthy lifestyle advice she found in her research.
Always willing to try anything if it had even the remotest chance of helping, Jamie decided to seek advice from a psychologist. She understood that psychologists undergo more extensive education and training than that of mental health counselors, which might allow them to shed more insight into her anxiety disorder.
Jamie began seeing Dr. Knight, a psychologist. At their second meeting, Jamie had brought along some research she had come across. When she attempted to ask questions about this research, instead of addressing her concerns or entering into a conversation with her, this psychologist, sarcastically and with a smirky smile, responded, “Why would you ask these questions? You're not a psychologist.” Nor was he interested in discussing any of the other information in the books she had brought along.
After her third appointment with Dr. Knight, Jamie realized that his insights and guidance were no more in-depth than the advice she had been reading in "How to Handle Stress" articles from magazines she had picked up at the grocery store. After seeing no positive results from their sessions, Jamie decided there was no reason to continue seeing Dr. Knight.
Chapter 37 New Symptoms
It was around this time that Jamie developed compulsive behaviors. She had continued to stay on most of the healthy eating guidelines outlined in the Functional Medicine diet, but now found herself hoarding food. Fearful she wouldn’t have enough options for healthy meals, she began cooking and freezing food, filling her freezer to its full capacity, way beyond what an average person would ever use.
And then there was her extreme fear of gum recession. She began checking her gums by pulling back her lip and getting up close to the mirror to examine them. This checking escalated to over 10 to 20 times a day. It got so bad that she stopped turning on the bathroom light, preventing her from seeing her gums.
This behavior continued for about a year and a half. Even at her six-month dental appointments, when the dentist assured her that her gums were very healthy and saw absolutely no problems, it didn’t stop her from obsessing over them.
Over the years, Jamie still, if not vigilant, can be susceptible to developing new obsessions. Invariably, as she puts one to rest, there always seems to be another that will emerge.
Shortly after her disappointing experience with Dr. Knight, Jamie began experiencing night terrors, waking up in the middle of the night and struggling to breathe. She was having panic attacks in her sleep.
Exhausted from work and lack of sleep, she felt compelled to consult yet another psychiatrist, Dr. Barry.
On her first appointment with Dr Barry, Jamie presented a list of the previously unsuccessful drugs she had been prescribed. Dr. Barry took a few minutes to study her drug list, then looked up at Jamie and said, “You haven’t been on that many drugs.” Jamie is sitting there, not believing what she just heard. More than 20 different prescriptions had been tried, and some retried, and this doctor was telling her she hadn’t been on that many drugs!
Dr. Barry provided no information about the treatment plan she intended to implement. Jamie viewed the situation as yet another doctor randomly prescribing drugs to see which one might stick. Which meant weathering through more side effects and more withdrawal symptoms. Frustrated, Jamie decided she had had enough and walked out, and never returned.
If she had been diagnosed with a severe disease, people would have been falling all over themselves with “I’m so sorry,” condolences, and assurances that they were going to do everything possible to help her. Again, I have to say, if they couldn’t see it in a blood test or on an X-ray, they couldn’t understand what Jamie was dealing with.
Between the ages of thirteen and twenty-nine, Jamie had met with ten different counselors, seven psychiatrists, and two psychologists. Some were warm and compassionate, while others didn’t know how to help her, and a few had been negative and unsupportive.
Jamie wondered if she wasn’t doing enough to help herself or if the help she needed simply didn’t exist, and no one was willing to admit it to her.
Chapter 38 More Pieces Of The Puzzle.
After the failed meeting with the latest psychiatrist, Jamie made an appointment with a new primary doctor, Dr. Andrews, an internal specialist. Seeking her advice, Jamie asked her what to do and where to go next.
Dr. Andrews sat patiently listening to her story, and after reviewing all the drugs she had been on, she began to see the whole picture; she surmised that Jamie’s emotional upheaval could be hormonal, and her anxiety could be blamed on a lack of healthy levels of serotonin in her brain.
From Jamie’s answers to her questions, Dr. Andrews came up with a simple plan; A low dose of Loestrin MG, a birth control pill, for hormonal balance, and a low dose of Zoloft to help balance serotonin levels (both of these drugs had been tried in the past but not in this combination).
Dr. Andrews also referred Jamie to an OB-GYN, an obstetrician-gynecologist specializing in female reproductive health, for a consultation on hormone therapy.
The OB-GYN agreed with Dr. Andrews that this combination of drugs could possibly help with managing Jamie’s GAD.
Dr. Andrews also suggested that Jamie see a cardiac physician to revisit her POTS diagnosis and referred her to Dr. Green.
Dr. Green, a cardiologist, was ‘exactly what the doctor ordered.’ He was warm and funny, explaining that he could probably help her, but assured her he had an excellent referral to send her if he couldn't.
When Jamie had been diagnosed with POTS years ago, she was never told how or what she should do to live with it. Dr. Green had a simple, straightforward solution: He told her to increase her salt intake to maintain her body’s fluid volume, which should alleviate lightheadedness whenever she stands up. Do not sit or stand too long at a time or get up and down too quickly. Do not let yourself get overheated. Eat small meals throughout the day. Lastly, build up your core muscles.
Jamie came home, started adding extra salt to her meals, and incorporated daily exercises to develop core muscles. The POTS symptoms have mostly disappeared over time; however, persistent weakness in her lower legs remains, preventing her from standing longer than ten or fifteen minutes at a time.
Thanks to Dr. Green's suggestions, she can now take short walks to enjoy the fresh air and sunshine again.
It wasn't long before I could see that the medications prescribed by Dr. Andrews were helping Jamie. While they did not completely eliminate her anxiety, they enabled her to manage it more effectively. She noticed that her racing thoughts began to slow down, allowing her to practice calming meditation exercises in the evenings. During the day, whenever stress threatens to overwhelm her, she engages in mental distractions, such as reading or journaling, to help relieve it.
Chapter 39 Living With Anxiety
When I feel anxious, I stop and ask myself why, and I can usually identify the reason, such as going to the dentist or being overcharged on a bill. But Jamie lives with a brain that doesn’t always make sense and can’t always recognize what’s real or what’s not.
During one of her therapy sessions, Jamie learned that a panic attack can trick her brain into believing that something is happening in the moment, such as imagining a tiger attacking her. Her brain doesn't understand that it's just a thought.
Whenever Jamie experiences anxious thoughts, she consciously reassures herself that they are simply thoughts and that, with relaxation techniques, they will pass. This is a long way from the days years ago, talking for hours on the phone, processing every scary thought her GAD creates.
With her PD, panic disorder, sometimes, no matter what Jamie does, panic attacks still appear without warning. The major difference now is that she understands they are not her fault, and no longer beats herself up for being weak for the inability to control them as she had in the past.
Over the years, Jamie has learned various coping techniques, one of which is called Tensing. This technique involves simultaneously tightening every muscle in her body, from her face to her toes, and holding the tension for several seconds. Jamie doesn’t like tensing, but she does it anyway because it does help dissipate her physical anxiety symptoms.
Never willing to settle, Jamie attended a two-day seminar in Chicago on ‘Meditation, Mindfulness, and Emotional Intelligence’ to learn more in-depth calming techniques. She now incorporates daily deep breathing exercises, takes walks, healthy meal planning, and makes sure to get a good night's sleep. She has learned that letting herself get too tired or too hungry can set her up to be more vulnerable to elevated stress levels.
Chapter 40 Then Came Covid
When I retired, I moved to be near Jamie. Since we have such a close relationship, she decided to let her apartment go and move in with me. We both looked forward to being roomies again, as we have always enjoyed each other’s company. Boy, was I glad when COVID-19 hit that we had each other.
Jamie struggled with her anxiety, just like many of us did, during that difficult time. I myself escaped into TV programs and books. But, of course, Jamie’s GAD escalated, and her OCD went into overdrive. From everything we saw on the news of people dying and the medical field helpless to help them, Jamie became obsessively germophobic. She wouldn’t let anyone come into our home, even if they wore a mask. We only ordered delivery food once; she was so obsessed that she requested ‘no contact’ delivery, telling them to leave our order at the door, and then went crazy sanitizing the packaging it came in. I admit I was a little ‘nutso,’ too, but not at the level Jamie suffered from.
During the worst part of the COVID-19 pandemic, Jamie's film department closed down, and it was months before they reopened. When everything returned to normal, Jamie was called back to resume regular office hours. At age 31, after working only five years in the hospital’s film department, she quit.
During the time Jamie was out of the office, she had developed a new debilitating symptom: fatigue. It started out slowly in the beginning. First, she began sleeping ten to twelve hours a night and then progressed to adding a two to three-hour nap every afternoon.
Struggling with fatigue and the energy drain caused by her anxiety, Jamie found simple tasks such as eating, dressing, and driving the forty-five minutes to work too overwhelming. By the time she reached her desk in the morning, she was already too exhausted to put in a full day’s work, and the thought of facing the long commute home was equally daunting. The only option was to let her job go.
At the beginning of the pandemic, we both suspected we had contracted a mild case of COVID-19. Later, as research emerged about long-term COVID-19, the doctors questioned whether this could have triggered Jamie’s increased fatigue.
So, back to the drawing board.
Part 3
Chapter 41 New Diagnosis
Jamie started a new search for answers to her fatigue problem, beginning with a visit to her primary care physician, Dr. Andrews.
Dr. Andrews first thought she might have a disorder called sleep apnea, a condition that prevents her from getting adequate oxygen at night, contributing to her exhaustion during the day. She referred Jamie to a sleep clinic.
The sleep clinic evaluation ruled out sleep apnea and instead diagnosed her with chronic fatigue syndrome, CFS.
The frustrating part of this condition, as we were to learn, is that the medical field has yet to figure out how to treat CFS.
Dr. Andrews's only advice was to consult the Functional Medicine Department. When Jamie told her she had already been through their program, Dr. Andrews then referred her to a psychiatrist to revisit her GAD.
Her new psychiatrist, Dr. Day, confirmed her diagnosis of PD (Panic disorder, a condition in which your body goes into a panic attack at any given moment with or without cause) and OCD (Obsessive-compulsive disorder, characterized by uncontrollable repetition of the same thoughts and behaviors). Jamie already knew about the PD, and through her own research, had suspected she suffered from OCD.
Dr. Day also officially diagnosed Jamie with PMDD, premenstrual dysphoric disorder, a condition that causes severe physical and emotional symptoms a week or two before a menstrual cycle.
When Dr. Day talked about PMDD symptoms, it sounded exactly like Jamie’s anxiety-driven, unpredictable moods. To manage these intense emotional upsets, Dr. Day recommended increasing her Zoloft dosage at the moment of their onset.
Thankfully, Dr. Day’s recommendation to increase her Zoloft has significantly helped when Jamie finds herself in one of her sudden, weepy, crying states.
The most serious symptom left to deal with is the exhaustion. We always knew that living with anxiety takes a lot out of Jamie; however, the chronic fatigue syndrome diagnosis is an entirely different story.
Dr. Day referred Jamie to a rehabilitation center, to meet with a physical therapist to learn more about living with CFS.
The therapist began by introducing a gentle exercise program that accommodates her POTS condition and incorporating short walks into her routine. Jamie learned that managing chronic fatigue syndrome is all about learning how to pace yourself. If she overdoes it one day, she finds it’s often followed by a day or two of low energy and excessive sleeping until she recovers.
Jamie returned to her heart doctor, who, upon hearing about her struggles with CFS, recommended a drug called Fludrocortisone, sometimes used to manage POTS, hoping it would help with her energy, but it did nothing. He then prescribed Midodrine, a drug used to treat low blood pressure, but this drug aggravated her anxiety.
Again, she found that drugs were not the answer.
Chapter 42 Living With Chronic Fatigue Syndrome
Jamie usually has about two to three hours of energy most mornings. By lunchtime, she usually fizzles out and ends up lying on the couch quietly reading or watching TV. By early evening, she might experience another short burst of energy before bedtime. She sleeps an average of eleven hours a night, and two or three times a week, needs a long nap in the afternoon.
I see how down and frustrated Jamie gets sometimes. After all the years of battling anxiety and finally being in a good place managing it, she now has to contend with chronic fatigue. But don’t get me wrong, Jamie still considers herself lucky. She recognizes that there are people in far more dire situations than what she finds herself in. It's common for her to comment on how grateful she is for all the support she receives.
Dr. Day, in the pursuit of getting Jamie back to work and not wanting to overlook anything, referred Jamie to a muscular neurologist for chronic fatigue.
The muscular neurologist reviewed Jamie’s test results and immediately noticed that her blood test indicated she was deficient in vitamins D and B12. She suspected this could contribute to some of Jamie’s fatigue and suggested supplements to increase these vitamin levels.
When Jamie’s vitamin D and B12 levels returned to normal, her energy level did not improve, leaving her uncertain about what to do next.
Chapter 43 Keeping Busy
After resigning from her editing position at the hospital, Jamie began searching for alternative work that she could do from home. She taught herself to build websites and has become interested in graphic design. Also returning to her love of writing, she has written several short stories and anecdotes about living with GAD, and posted them on her website.
Screenwriting was one of Jamie’s favorite classes at college, not only enjoying them, but found she had a knack for it. She is presently working on developing some of her screenplay ideas and intends to use her film school connections, hoping to get her work considered for movies or TV shows.
I believe that the tiny seed planted years ago while watching the cartoon, she thought she could have made better, and her dream of working in the film industry still exists within her.
Chapter 44 Finally Caving.
For the past two years, I have been encouraging Jamie to file for disability. It was evident that with the CFS diagnosis being the final blow, it may take a while before she would be able to return to gainful employment.
Last year, at the age of 33, Jamie finally applied for disability. It has been difficult for her to accept the need for financial help. For someone as driven and independent as Jamie, to her, it means she is unable to support herself, and that’s a scary place for anyone to be in. She doesn’t bring it up very often, but I know she worries about what is going to happen to her.
Chapter 44 Renewed Hope Yet Again?
Recently, Jamie’s psychiatrist referred her to yet another specialist, a psychologist, Dr. West, who works specifically with patients with chronic illnesses.
Jamie thought she had turned over every stone there was to turn over in the medical field regarding her diagnoses, and believed that there would be little Dr. West could do for her.
Boy, were we surprised by the outcome of her meeting with her!
Dr. West presented a whole new plan. She believes, to put it simply, Jamie suffers from faulty brain wiring, and her POTS is responsible for this glitch.
Dr. West said that Jamie’s brain sends out faulty messages to all parts of her body, not just to her heart, but is also responsible for triggering her GAD, OCD, PMDD, PD, and CFS symptoms.
Dr. West recommended the hospital's Autonomic Program for Jamie to investigate how her faulty brain wiring affects her body’s functions and gain a deeper understanding of her diagnosis.
In this program, specialists examine aspects and functions of Jamie’s bodily systems. An internal specialist on POTS, an OB-GYN specializing in POTS' impact on estrogen and progestin levels, and enrolled her in virtual educational classes on living with chronic fatigue, POTS, GAD, and OCD.
When Jamie met with the internal specialist, Dr. Yost, she learned about a drug called LDN (Naltrexone), which may help with her fatigue. Research shows it has been helpful in treating people with long COVID symptoms.
Initially, this drug has been used to help people suffering from opioid addiction, but for Jamie’s condition, the dosage is approximately one-tenth of the dose that is given to an addict.
Dr. Yost also gave an explanation for Jamie’s Chronic Fatigue Syndrome. He believes Jamie had a virus in the past that could have caused CFS, and even though the virus has cleared her system, it may have left behind inflammation. This could be the source of her fatigue, and LDN could have a good chance of clearing out this inflammation, returning her energy.
Although Jamie has only been on this drug for a short time, she hasn’t seen much of a difference in her symptoms. She has, however, noticed some of her OCD tendencies have lessened, and the insatiable eating sensation she still had been experiencing quite often over the years since being on the Functional Medicine Diet has subsided. But for me, I have noticed one REALLY BIG CHANGE: her sense of humor has returned.
The long years of struggling with her diagnosis had taken the joy out of Jamie, but now I can see it slowly returning. At the age of 34, I hadn’t realized how much Jamie’s sense of humor had been missing until a couple of days ago when I found us both hysterically laughing over some silly little thing.
As the weeks pass, it's becoming more and more common to hear Jamie’s laughter and see her smiling more easily. This was part of her personality that I hadn’t seen since her early days of middle school before she was diagnosed with GAD at age 13.
After three years of staying at home, this week, she accepted two social invitations, overcame her social anxiety, and attended both of them. The potential benefits of this LDN drug feel like it could be the light at the end of a very long tunnel, but it will still take several months before Jamie has the answer.
Chapter 45 Good News And Bad News
The bad news is that, after months of being on LDN, Jamie met with Dr. Yost and reported that she saw little change in her energy level. Dr. Yost said it had been long enough that she should have seen results by now. He did say that some of his patients saw a better response when he raised the dosage to 6mg. He told her if that was the case for her, there was a good chance she would see better results.
With fingers crossed, we hope that will be the case. But, again, we were told it would take months to see the outcome and to be patient.
The good news, Jamie was approved for full disability benefits. She will receive financial support for the next three years until her next review is due. This significantly reduces the emotional burden she has been carrying, allowing her to fully focus on her health and the goal of eventually return to work.
Final Thoughts
Over the years, Jamie has faced countless obstacles and endured many moments of uncertainty, but her determination has never wavered. I often marvel at how she battled through all the tough times, unaware of how bad things were going to get or that they would go on for years. She lived it day by day, and I watched her face each day with inspiring inner strength and perseverance.
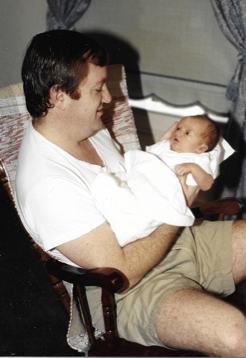
The End For Now
If you want to continue following our journey, check back; I will continue to post updates from time to time.
A Message From Jamie
The scariest thing about my mental illness is how powerful it can be. It takes over. Something inside my mind takes full control of my thinking, my words, and sometimes my actions. Then, it sends out messages to my body, putting me in a state of panic. It feels like a vice is squeezing my chest. I struggle to breathe, my world turns upside down, and I find myself in a confused mental state, unable to make sense of anything. And then a deep sense of dread washes over me, knowing that there is no escape from what is happening to me at the moment.
Was this a good description of a panic attack? No, it’s not even close, but it’s the best I could do. I have yet to find the words to tell another person the overwhelming sensations I experience in a full-blown panic attack. I have learned techniques to help shorten the length of most of my attacks. However, no matter what I do, I know that, in all probability, there will always be another one waiting around the corner to emerge unexpectedly at any time.
It’s different today. Through education and understanding, I know what is happening in my brain, and although I have been able to take the scary ‘I think I’m dying’ away during an attack, they can still feel just as devastating as ever.
I define my success in living with my diagnoses as finally accepting that they are not my fault. I did not create these conditions; I inherited them. While this may seem obvious to most people reading my story, in the early years of my illness, I was obsessed with the idea of finding a cure.
It took me years to accept my circumstances. When I finally realized that I needed to get over myself, buckle down, and start learning how to live with my illnesses, they became more bearable.
Accepting my situation doesn’t mean I‘ve given up or settled, far from it. It just means I work very hard with what I know to make each day the best it can be. In the meantime, I patiently wait for the medical field to catch up, developing new research and treatments to further help people like me.
Jamie Miller
If you would like to follow Jamie’s writing, visit her website lifeplusanxiety.com, where she continues to post short stories for young adults and personal stories about living with generalized anxiety.
Why I Dedicated This Story To Lois Miller
From the information Jamie gave Dr. Baker at that first visit at Integrated Medicine about having an aunt who spent time in a mental institution, led her to suspect Jamie had inherited mutated genes. I cannot express enough how that information changed everything for Jamie. It was as if the world opened up to her. She realized she wasn’t a freak; she wasn’t imagining or creating her anxiety. It was real; it was tangible.
Jamie grew up hearing stories about her Aunt Lois. Lois was a troubled teenager, and in the 1950s, her parents admitted her to a mental hospital. Jamie’s father, Jim, had talked to me about how scared he was the night they drove to the hospital. He was five years old, and Lois was 19; he described her as being very angry and out of control.
The situation was terrifying for him. So terrifying, in fact, that early in our relationship, he told me he was reluctant to have children for fear of passing on the mental illness he had seen in his sister. Which I think is a strong testament to the horrific scene he must have witnessed as a child.
Of course, when he told me this, I immediately dismissed it, believing Lois’s condition was an isolated case. No other family members showed signs of having such a mental illness.
Jim's older sister, Edna, who was four years Lois’s junior, despised Lois. She described their household as being in a constant state of volatility, and fighting between Lois and her other family members.
Jim’s older brother, Harry, was two years older than Lois. After we learned about Jamie’s mutated genes, I talked to Harry to gather background information on the Millers’ side of the family. He told me at the time of Lois’s admittance to the mental institution, she had been diagnosed with Pathological Anxiety.
By the 1950s, the medical field had begun to develop psychotropic drugs used to help calm down anxious and aggressive behavior. These drugs helped replace the physical restraints that, up until then, had been used in controlling patients and protecting their caregivers from injury. I can only hope Lois was able to receive drugs and avoid the unimaginable, traumatic horrors of being strapped down.
When I went through school for my mental health degree, I learned that the mental health system we have today did not exist in the 1950s. The ‘Mental Health Movement’ began with President John Kennedy’s administration. In 1963, President Kennedy signed a bill to establish outpatient mental health centers nationwide. Today, every county in the United States has one of these centers where anyone can walk in and ask for help. Sad to say, these centers were not available in the early l950s for Lois and her family.
So, what happened to Lois? After being admitted to the hospital that night, she was never allowed to return home again. In fact, the family pretty much forgot about her. Years later, Edna even omitted her name from the list of family members in their father’s obituary as a surviving daughter.
According to Harry, Lois eventually left the hospital, found work in a factory, and was even able to purchase a home. However, in the 1970s, Harry heard she had quit her job and lost her home.
The next time the family heard from Lois was a late-night phone call from the police department. Lois had been taken into custody for causing a public disturbance, and they were asking for someone to come and pick her up at the police station.
Edna and Harry both discouraged their father from going. As a result, since there was no one to care for her, Lois ended up in the county home’s psychiatric floor. She stayed there for several years until she was transferred to a group home, where she lived out her final days and died from a heart condition at the age of 63.
I do not fault Lois’s father for not going to the police station that night. At the time, he was not in a position to help his daughter. He was elderly, and Lois’s mother had already passed away. Harry and Edna wanted nothing to do with her, having lived through the nightmare years long ago before she was removed from the home.
As a mother, it scares me to think that Lois’s story could have been my daughter’s story if Jamie had been born years earlier, before the mental health help we have today had not been available to her. Still, there were times when her emotions were so out of control that it’s a wonder she hadn’t ended up in a psychiatric ward unit.
I know how hard it would have been for the Miller family to be overwhelmed and feel defeated with their daughter, Lois. I had felt that way so many times during those days when I received phone call after phone call, day after day, from Jamie while she was away at college. She was constantly seeking my help to talk her down from the latest crisis her brain was creating. Sometimes, I wonder how I managed to keep my own sanity, and there were times when I almost lost it. But I knew during those times what I felt was just the tip of the iceberg compared to what Jamie was experiencing.
Those were very dark days for us; no, I cannot blame Lois’s family because, as I have said earlier, I have an associate's degree in mental health. When I worked as a drug and alcohol abuse counselor, I had the counseling skills needed to work with someone like Jamie. My training included communication techniques referred to as ‘helping skills,’ as well as training in crisis counseling that all mental health professionals are expected to learn. Still, I was helpless to help Jamie. Her condition was far beyond what talk therapy could do.
Fortunately, I had moved on from the counseling profession and opened a home business, allowing me to be available to Jamie whenever she needed me most. I will always be eternally grateful for the school counselors who were there when I couldn’t be, to pull her back time and time again when she was in danger of going over the edge.
Jamie often thinks about her Aunt Lois and feels a deep sense of empathy when imagining the emotional trauma her aunt must have endured. She wonders how she herself would have coped if left all alone in a mental hospital.
Being very aware herself of how intense and terrifying anxiety can be, Jamie can only imagine how overwhelmingly helpless her aunt must have felt.
After reading Lois’s story, you may understand why I dedicated this story to her. Every time I reread it, I still get emotional about what she must have gone through. Jamie and I took the opportunity to visit the mental hospital where Lois had spent time. Driving up the long, winding road to the menacing-looking main building really brought home the reality of that fateful night long ago and what Lois would have experienced.
My final words are to simply say,
“ Rest in peace, my dear Lois. You will always be remembered.”

I would love to hear your feedback by contacting me at contact@lifeplusanxiety.com. Thank you for reading my story.
